The CMS Spring Conference Has Come and Gone!
The Centers for Medicare & Medicaid Services (CMS) held its annual spring conference, and although it was a shortened conference this year with four areas of discussion as well as a keynote address by Demetrios Kouzoukas, Principal Deputy Administrator for Medicare and Director of the Center for Medicare, they did cover some important changes about which many plans should be thinking and preparing.
Medicare Advantage (MA) Value-Based Insurance Design (VBID) Model Update
As part of its goals for the 2020 MA VBID Model, CMS is testing concepts for modernizing MA health plans. CMS did this by soliciting comments from beneficiaries, increasing the value of Reward & Incentive (R&I) programs to $600 per year, including Part D in the 2020 R&I programs, and developing telehealth intervention in rural and underserved areas.
A potential big change will be tested in calendar year 2021 when CMS plans to add the Medicare hospice benefit into the MA VBID Model. By doing so, CMS hopes to see an increase in quality and access to care while fostering partnerships between Medicare Advantage Organizations (MAOs) and hospice providers. The MAO will be the point of accountability and function as the hub to ensure access to a seamless continuum of care. Some important factors CMS is looking to address include the following:
- Respite benefits for caregivers
- Continuous level of care
- Creating opportunities for innovation
- Monitoring to ensure appropriate and high-quality care
Additionally, CMS discussed key policy considerations for 2021 VBID:
- How to ensure beneficiaries still have the ability to go to a particular hospice
- How payment will work between plans and CMS
- Evaluate and look at cost and quality
CMS will be scheduling webinars for those interested in participating, providing an opportunity to help with the design of the pilot.
New Medicare-Medicaid Integration Policies
The Bipartisan Budget Act of 2018 (BBA) requires a minimum level of Medicare-Medicaid integration for all applicable Dual-Eligible Special Needs Plans (D-SNPs). These D-SNPs must meet one of the following criteria by 2021:
- Be a Fully Integrated Dual Eligible (FIDE) SNP
- Be a Highly Integrated Dual Eligible (HIDE) SNP
- Notify the state or its designee(s) of hospital and skilled nursing facility (SNF) inpatient admissions for certain high-risk enrollees
CMS defines an “applicable integrated plan” as a FIDE/HIDE SNP with exclusively aligned enrollment and the Medicaid managed care organization through which one of the following entities covers Medicaid services for D-SNP enrollees:
- The D-SNP; or
- The D-SNP’s parent organization; or
- Another entity that is owned and controlled by the D-SNP’s parent organization.
Intermediate sanctions will be imposed during plan years 2021 through 2025 for those MAOs with a D-SNP contract not meeting one of these three integration criteria.
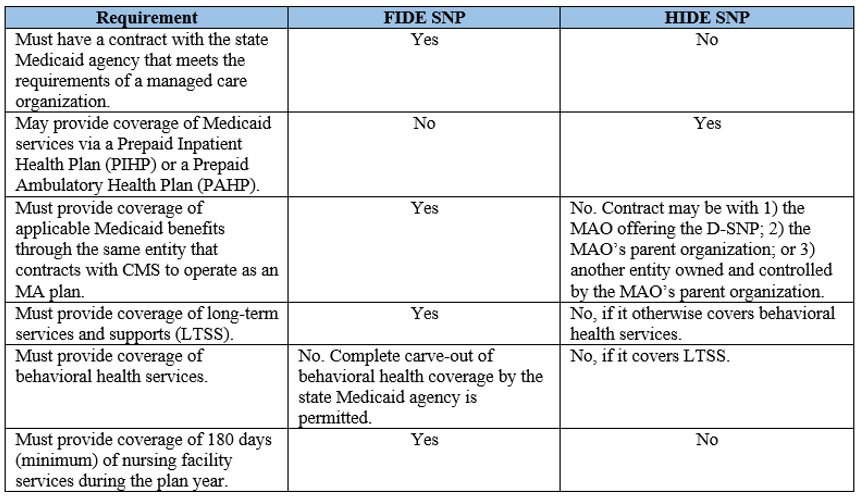
To explain the differences between FIDE and HIDE, CMS outlined the following:
The final rule establishes that all applicable integrated D-SNPs must assist members with Medicaid coverage and appeals and grievances. While appeals and grievances have been separate systems between Medicaid and MA since the beginning of time, the BBA is requiring a unified appeals and grievances procedure in 2021, including provision of continuing benefits while an appeal is pending. This, along with no deadline for filing a grievance, is likely a big change for MAOs who should start planning now for the needed changes to processes and systems.
CMS recommends starting your planning now. Work with your respective states, revise state Medicaid agency contracts, and start working out the operational and procedural changes for a unified appeals and grievances process.
If you weren’t able to attend in person or via the web, you can access the conference materials here. Also, be sure to check out the Integrated Care Resource Center at: https://www.integratedcareresourcecenter.com/.
Resources:
Stay connected to industry news and gain perspective on how to navigate the latest issues through GHG’s weekly newsletter. Subscribe
Learn how a single platform designed specifically for Medicare can streamline enrollment and offer a better way to deliver a return on your plan’s investment. Click here
GHG Advisors is part of the Convey family of companies, which includes Convey Health Solutions, Pareto Intelligence, and HealthSmart International. Together, we collectively support healthcare organizations with elite consulting services and industry leading technology solutions. Learn more

